Steatotic liver disease - Causes & Treatment
Steatotic liver disease refers to disorders characterized by abnormal lipid accumulation in the liver (liver or hepatic steatosis). Steatotic liver disease includes what was previously known as non-alcoholic fatty liver disease (NAFLD), but is now referred to as metabolic dysfunction-associated steatotic liver disease. Steatotic liver disease also includes alcohol-related liver disease (ALD), MetALD, a new categorization for the overlap between MASLD and ALD, as well as unusual causes of liver steatosis.
Steatotic liver disease affects around 30% of the global population and is mostly caused by obesity, type 2 diabetes, and alcohol consumption; however, only a small fraction of those with steatotic liver disease develop cirrhosis. The presence and advancement of liver fibrosis caused by hepatic inflammation is the most reliable predictor of liver death across the whole range of steatotic liver disorders. A combination of recent advances in widely available biomarkers for early identification of liver fibrosis, as well as significant advances in treatment strategies, provides the opportunity to minimize morbidity and death in individuals with steatotic liver disease.
Fatty liver
Their are two types of fatty liver:
- Alcoholic fatty liver
- Non-alcoholic fatty liver
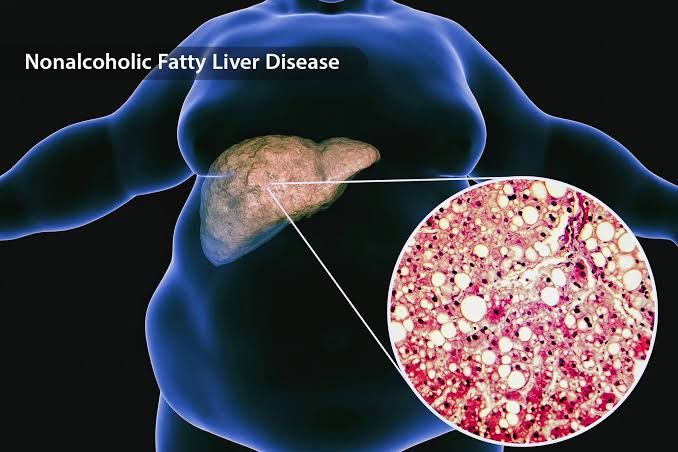
1. Non-alcoholic Fatty liver (NAFLD)
Non-alcoholic Fatty Liver Disease (NAFLD) or "Fatty Liver" is defined as the presence of macro vesicular alterations without inflammation (steatosis) and lobular inflammation in the absence of significant alcohol consumption. NAFL is described as hepatic steatosis without evidence of hepatocellular damage, such as ballooning of hepatocytes.
NAFLD is usually linked to Metabolic Syndrome, obesity, diabetes, and hyperlipidemia. Nearly 80% of people with Metabolic Syndrome have NAFLD.
NAFLD progresses through multiple stages, including simple steatosis, steatohepatitis, fibrosis, and cirrhosis, which can eventually lead to hepatocellular cancer. The disease progresses slowly; when steatosis is the only histological result, it is classified as a silent liver disease. Non-alcoholic steatohepatitis is defined by the presence of hepatic damage, inflammation, and/or fibrosis.
Fat accumulates in the liver for a variety reasons. It is most usually associated with increased transport of free fatty acids to the liver, increased synthesis of fatty acids in the liver, decreased oxidation of FFA, or decreased synthesis or secretion of very-low-density lipoprotein. Oxidative stress in hepatocytes activates stellate cells, leading to collagen synthesis and inflammation. Other variables that may lead to fatty liver are:
- The usage of specific drugs
- Metabolic anomalies (such as glycogen storage disorders and homocystinuria)
- Alcohol consumption - Nutritional status (e.g., total parenteral nutrition, severe malnutrition, overnutrition, or starvation diet).
- Other health conditions, such as Wilson disease and celiac sprue.
Causes of NAFLD
Insulin resistance is currently thought to be the major metabolic abnormality that causes NAFLD. Insulin resistance promotes the uptake of free fatty acids into the liver. This occurs when insulin fails to regulate the hormone-sensitive lipase, allowing more FFA to be produced from adipose tissue. Furthermore, higher insulin levels and insulin resistance enhance the ongoing synthesis of triglycerides in the liver. These two sources of triglycerides cause fat buildup in hepatocytes, which leads to macro vesicular hepatic steatosis.
Non-alcoholic fatty liver disease (NAFLD) prevalence is quickly increasing, particularly in Western countries. Rising obesity rates, an increase in childhood obesity, sedentary lifestyles, consumption of unhealthy fast food, and a longer lifespan are all possible causes. The incidence and prevalence of NAFLD are underestimated since ultrasonography is routinely employed to detect fatty liver disease. NAFLD affects 80% to 90% of obese adults, 30% to 50% of diabetics, 90% or more of those with hyperlipidemia, 3 to 10% of children, and up to 40% to 70% of children who are obese.
The treatment focuses mostly on lifestyle changes and weight loss. Treatment includes hyperglycemia and lipid control. Gastric bypass surgery or other weight loss procedures should be explored for patients with severe obesity. Weight loss has been shown to reduce hepatic steatosis. According to the data, a steatosis improvement requires a 3% to 5% weight loss.
The difficulties associated with fatty liver are as follows:
- Cirrhosis
- Ascites
- Esophageal varices
- Liver failure
- Liver cancer
- Type 2 diabetes
Obesity is another factor that contributes to NAFLD. Obesity raises the risk and severity of non-alcoholic fatty liver disease (NAFLD), which is defined by excessive fat accumulation in the liver that is not induced by alcohol consumption. Obesity, particularly visceral adiposity (fat around abdominal organs), causes an increase in free fatty acid (FFA) flow to the liver via the portal vein. This exceeds the liver's ability to process fats, resulting in triglyceride accumulation (steatosis), which is a hallmark of NAFLD. Furthermore, excess fat in the liver causes inflammation (lipotoxicity) and oxidative stress, which can develop NAFLD to non-alcoholic steatohepatitis (NASH), a more severe form of liver inflammation and damage. Furthermore, obesity is significantly associated with insulin resistance, a major cause of NAFLD. Insulin resistance disrupts glucose and lipid metabolism, increasing lipogenesis (fat synthesis) in hepatocytes and decreasing fat export from the liver. NAFLD is quite common in obese people, with studies showing that 70-90% of obese adults have some kind of liver steatosis. The risk rises with increasing body mass index (BMI).
2. Fibrosis
Fibrosis occurs when the liver produces scar tissue as a result of chronic damage or inflammation. Think of the liver as a tireless organ that cleans your blood, aids digestion, and stores energy. When the liver is injured—by things like obesity, excessive alcohol consumption, or disorders like NAFLD (non-alcoholic fatty liver disease), it attempts to repair itself. This repair process produces stiff, fibrous scar tissue that resembles patches on a worn-out tire. Over time, these scars stiffen the liver and impair its ability to operate normally.
The health consequences for the liver are severe. Mild fibrosis may not create any visible difficulties, but as scars accumulate, the liver's capacity to filter toxins, digest nutrients, and make essential proteins deteriorates. This can result in weariness, edema, or jaundice (yellow skin). If left untreated, fibrosis can proceed to cirrhosis, a more serious condition in which the liver becomes severely damaged and may fail. Fibrosis also increases the chance of liver cancer and problems such as portal hypertension, which occurs when blood flow is impeded and vein pressure rises, potentially leading to bleeding. Early fibrosis can be reversed with lifestyle modifications, such as weight loss in obesity, but advanced stages are more difficult to cure and may require medical intervention.
3. Cirrhosis
Cirrhosis is a devastating liver disease in which good liver tissue is replaced with scar tissue over time. Consider the liver, which functions as a filter, purifying your blood and aiding digestion, becoming stiff and lumpy owing to long-term damage. Obesity, excessive alcohol consumption, and chronic liver illnesses such as NAFLD (non-alcoholic fatty liver disease) can all cause scarring. As scar tissue accumulates, the liver fails to perform its functions properly.
The health implications for the liver are severe. A damaged liver is incapable of adequately filtering toxins from the blood, processing nutrients, or producing proteins required for clotting and fighting infections. This causes symptoms such as yellow skin (jaundice), swelling in the legs or abdomen, and easy bruising. Cirrhosis can also lead to serious problems, such as liver failure (when the liver stops working) or liver cancer. Blood flow through the liver becomes clogged, increasing pressure in veins (portal hypertension), which can result in serious bleeding. While early cirrhosis can be treated by lifestyle modifications or therapy, severe cases can be life-threatening, necessitating a liver transplant. Obesity exacerbates cirrhosis by promoting inflammation and fat accumulation, which accelerates liver damage.
Stages of Non-Alcoholic Fatty Liver Disease (NAFLD):
- Simple Steatosis (Fatty Liver): Fat accumulates in liver cells without causing severe inflammation or injury. It's usually asymptomatic and reversible with lifestyle adjustments.
- Non-Alcoholic Steatohepatitis (NASH): Fat accumulation is associated with inflammation and liver cell destruction. If not addressed, this stage can lead to more serious liver problems.
- Fibrosis: Persistent inflammation causes scar tissue growth in the liver. Liver function may remain normal, but the risk of advancement increases.
- Cirrhosis: Extensive scarring replaces good liver tissue, substantially reducing function. It is irreversible and can result in liver failure or cancer.
Therapies for non-alcoholic fatty liver disease
MASLD, or metabolic dysfunction-associated steatotic liver disease, is the new name for what was formerly known as NAFLD. It's a common condition in which extra fat accumulates in the liver and is frequently associated with being overweight, obese, or having a certain lifestyle. The good news is that MASLD may typically be reversed or treated well with easy, consistent lifestyle adjustments.
- Weight Management
Overweight or Obese:
- Aim to lose at least 5% of your weight to reduce fat in the liver.
- If you have more advanced liver issues (like MASH or fibrosis), try for 7–10% weight loss.
Healthy Diet
- Eating like the Mediterranean diet: lots of vegetables, fruits, whole grains, olive oil, nuts, and fish.
- Cutting back on:
- Processed meats
- Sugary drinks
- Packaged junk food
- Choose whole and minimally processed foods.
Physical Activity
- Moving our body! Aim for:
150 minutes/week of moderate exercise (like brisk walking)
OR
75 minutes/week of more intense activity (like jogging or swimming)
Try to sit less and be more active throughout the day.
Other Healthy Habits
- Avoid smoking
- Limit or stop alcohol, especially if the liver is already damaged
How to Make All This Work
- Working with a team of experts (doctors, dietitians, etc.)
- Talking about our lifestyle during check-ups.
- Joining affordable programs that help with healthy eating and exercise.
- Making a custom plan that fits our budget and routine.
- Using behavioral therapy if needed to stay motivated.
Prevention Tips
Even if one doesn’t have MASLD or want to prevent it from worsening:
- Maintain a healthy weight
- Eat well
- Stay active
- Avoid smoking and limit alcohol
The ultimate goals of these lifestyle changes extend beyond liver health. They improve quality of life, increase survival rates, and provide considerable cardiometabolic benefits, such as a reduced risk of heart disease, type 2 diabetes (T2D), cirrhosis, and even liver cancer (HCC).
Link to the Research Papers:










Comments
Post a Comment