Excretory System
Excretion is the process by which metabolic waste products are removed (completely or partially) from an animal's body. It differs from egestion, which is the removal of undigested food materials from the body. Nitrogenous wastes (such as ammonia, urea, and uric acid) are the most major metabolic waste produced by mammals. These wastes are formed during the breakdown of amino acids and nucleic acids and are extremely hazardous to the cellular environment. The nature of nitrogen-containing wastes (ammonia, urea, and uric acid) and their excretion differs between species, depending on the availability of water. Ammonia is the most toxic type and requires a substantial amount of water to be eliminated, whereas uric acid, which is the least harmful, may be removed with minimal water loss.
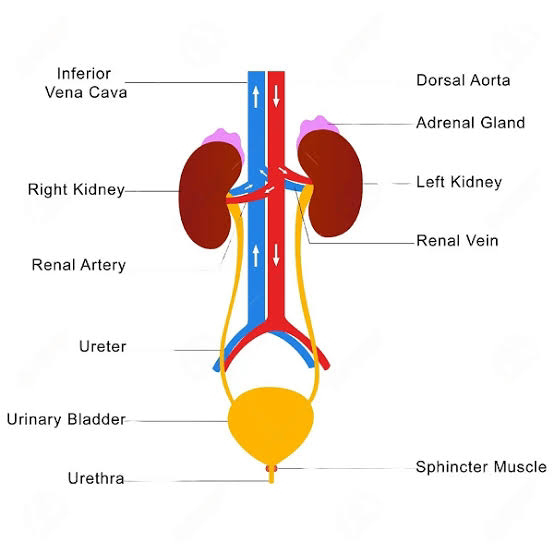
The human excretory system is made up of two kidneys, two ureters, one urine bladder, and a urethra. The kidney is a urine-producing organ. A renal artery supplies blood to each kidney, which then produces urine. Urine exits each kidney via a duct known as the ureter. Both ureters flow into the same urine bladder. The urinary bladder briefly retains pee. During urination, urine exits the bladder via a tube known as the urethra.
Functions of the Kidneys
The kidneys are the major organs of excretion, particularly for nitrogenous wastes. The kidneys are also important homeostatic organs because they manage the blood's water-salt and acid-base balances. The major functions of the kidney include the following:
- Regulation of water and electrolyte balance
- Regulation of blood Ph
- Regulation of arterial blood pressure
- Maintenace of blood osmolarity
- Secretion of hormones, erythropoietin
- Synthesis of enzyme renin
- Regulation of blood glucose level and glucogenesis
- Excretion of metabolic wastes such as urea, uric acid, creatinine through urine.
The kidneys are the principal organs responsible for removing metabolic waste products that the body no longer needs. These products include indude unsa (from amino acid metabolism), creatinine (from muscle creatine), uric acid (from nutiesic acids), hemoglobin breakdown byproducts (such as bilirubin), and hormone metabolites. The kidneys also eliminate the majority of toxins and other foreign compounds that the body produces or consumes, such as pesticides, medications, and food additives.
Structure of the Kidneys
The paired kidneys are reddish bean-shaped organs located on the abdomen's posterior wall, outside the peritoneal cavity. The right kidney is positioned somewhat lower than the left. Each adult human kidney is 10-12 om long, 5-7 cm wide, and 2-3 cm thick, with an average weight of 120-170 g. A notch called the hilum is located at the center of the kidney's inner concave surface, through which the ureter, blood arteries, and nerves enter.
Anatomy of the kidneys:
Each kidney is surrounded by a thin but tough and transparent sheet of dense irregular connective tissue known as the renal capsule. A frontal incision of the kidney shows two separate regions: the renal cortex and the renal medulla. The renal cortex is the kidney's superficial outer layer. The renal medulla is a dark, reddish-brown inner area. It is made up of renal pyramids that are conical in shape. Each pyramid's base faces the renal cortex, while its apes (also known as a rersal papilla) point toward the renal hilum. Renal columns (also known as Bertimi colurrins) are sections of the renal cortex that stretch between renal pyramids. The renal cortex and renal pyramids of the renal medulla form the parenchyma (functional component) of the kidney.
The parenchyma houses the kidney's functioning components, known as nephrons. The renal pelvis is a large funnel-shaped area within the hilum that contains projections known as calyces. Each kidney has 8 to 18 minor calyces and 2-3 major calyces. A small calyx transports urine to a larger calyx. Urine drains from the main calyces into a single big cavity known as the renal pelvis before passing via the ureter to reach the urinary bladder.
Blood supply of the Kidneys:
Each kidney takes blood from a renal artery, which then produces urine. The renal artery separates into many segmental arteries that nourish the kidney's various segments (areas). Each segmental artery divides into many branches that enter the parenchyma and go through the renal columns between the renal pyramids as interlobar arteries. Arcuate arteries are branches of the interlobar arteries that emerge at the cortex-medulla junction. The arcuate arteries divide to form a network of interlobular arteries. Interlobular arteries enter the renal cortex and send out branches called afferent arterioles.
Each nephron receives an afferent arteriole, which splits into a tangled, ball-shaped capillary network known as the glomerulus. The glomerular capillaries then reconnect to form an efferent arteriole, which transports blood from the glomerulus. The efferent arteriole has a smaller diameter than the afferent arteriole. Glomerular capillaries differ from other capillaries in the body in that they are located between two arterioles rather than an arteriole and a venule. The efferent arterioles split to generate peritubular capillaries in the renal cortex.
The peritubular capillaries surround the renal tubules. The vasa recta is a specific part of the peritubular capillary system that descends into the medulla in parallel with the Henle loops before looping back along them and returning to the cortex. Thus, the kidneys have two types of capillaries: glomerular capillaries and peritubular capillaries. Each nephron contains an efferent arteriole that connects the two sets of capillaries. Blood from the peritubular capillaries flows into the venous system. Peritubular capillaries eventually connect to produce peritubular venules. The venous system begins with peritubular venules and progresses through interlobular veins, arcuate veins, interlobar veins, and eventually renal veins. Blood exits the kidney via a single renal vein, which emerges at the renal hilum and transports venous blood to the inferior vena cava. The kidneys have no segmental veins; instead, the interlobar veins join in the renal sinus to form the big renal vein.
Nephron
Nephrons are the functional units of the kidney. Each kidney has around 1 million nephrons that are held together by connective tissue. A nephron is made up of tubules and related tiny blood arteries. The nephron's tubular component is a hollow, fluid-filled tube composed of a single layer of epithelial cells. Each nephron is made up of two parts: a renal corpuscle (or malpighian body), which filters blood plasma, and a renal tubule, which receives the filtered fluid.
A renal corpuscle consists of two parts: the glomerulus (a tuft of capillaries generated by the afferent arteriole) and the Bowman's (or glomerular) capsule (a double-walled epithelial cup that encloses the glomerulus). The glomerular capillary membrane is similar to that of other capillaries, with the exception that it has three layers (rather than two): the fenestrated endothelium (a layer of simple squamous cells known as endothelial cells), a basement membrane, and a layer of epithelial cells (podocytes) surrounding the capillary basement membrane. Good plasma is filtered in the glomerular capsule before passing into the renal tubule.
The renal zubule is made up of a proximal tubule, a loop of Henle (nephron loop), and a distal tube. Proximal tubules are classified into two types: convoluted tubules and straight tubules. Convoluted indicates that the tubule is tightly coiled rather than straight. The distal tubules of many nephrons drain into a single collecting duct. In a nephron, the Henle loop connects the proximal and distal convoluted tubules. The Henle loop is made up of three functionally separate segments: thin descending, thin ascending, and thick ascending.
Cortical nephrons make up around 80-85% of all nephrons. The renal corpuscles in these nephrons are positioned in the outer renal cortex and contain a short Henle loop that extends only slightly into the medulla. In 20-30% of nephrons, renal corpuscles are located deep in the renal cortex (near to the medulla), and the Henle loop is quite lengthy and runs deep into the medulla. These are referred to as juxtamedullary nephrons. Every nephron has a juxtaglomerular apparatus. This structure is situated near the glomerulus of the nephron. It is a specific structure composed of the distal convoluted tubule and the glomerular afferent arteriole. The juxtaglomerular apparatus consists of three types of cells: juxtaglomerular cells on the walls of the afferent arteriole (which produce and store renin), macula densa cells in the distal convoluted tubule, and extraglomerular mesangial cells. The macula densa is a specific collection of epithelial cells in the distal tubules that makes intimate contact with the afferent and efferent arterioles. Mesangial cells are specialized smooth muscle cells that surround the glomerular capillary loops. The juxtaglomerular apparatus regulates blood pressure and glomerular filtration rate.
Urine formation
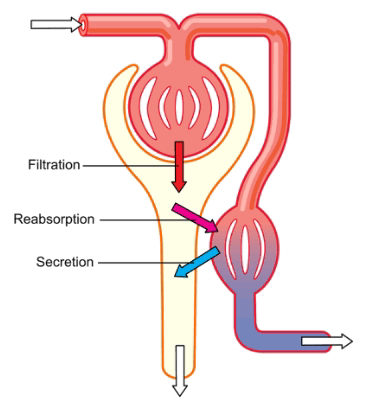
Nephrons and collecting ducts create urine through three main processes: glomerular filtration, tubular absorption, and tubular secretion. Glomerular filtration occurs within the renal corpuscle, while tubular reabsorption and secretion occur across the renal tubule and collecting duct.
1. Glomerular filtration
Glomerular filtration happens when blood enters the glomerulus via the afferent arteriole. Because of glomerular blood pressure, water and tiny solutes (such as glucose, amino acids, nitrogenous wastes, and lons) in blood flow from the glomerulus to the interior of the glomerular capsule. This is a filtering process because big molecules (such as proteins) and formed elements (blood cells and platelets) cannot flow through the capillary wall. The filtered fluid (known as the glomerular filtrate) is almost entirely protein-free and cell-free. Solute size has an inverse relationship with filterability. Adult males produce around 180 liters of glomerular filtrate each day. More than 99% of the glomerular filtrate is returned to the circulation by tubular reabsorption, leaving only 1-1.5 liters as urine.
The amount of filtrate generated in all renal corpuscles of both kidneys per minute is known as the glomerular filtration rate (GFR). A healthy person's GFR is approximately 125 ml/minute.
Regulation of glomerular filtration rate: Vasoconstriction or dilatation of afferent arterioles alters the rate of blood flow to the glomerulus, hence influencing glomerular filtration rate. Changes in the diameter of afferent arterioles are caused by both extrinsic and intrinsic regulating processes. These mechanisms are required to ensure that the GFR is high enough to allow the kidneys to remove wastes and regulate blood pressure while without causing excessive water loss. The three mechanisms that control GFR are brain regulation, renal autoregulation, and hormonal regulation.
Renal autoregulation of GFR: The kidneys have the capability to regulate GFR. This capability is called renal autoregulation. It involves two mechanisms- the myogenic constriction and tubuloglomerular feedback. These mechanisms are working together and maintaining nearly constant GFR over a wide range of systemic blood pressures.
Myogenic constriction of the afferent arteriole happens when the smooth muscle detects and responds to an increase in arterial pressure. As blood pressure rises, so does GFR due to increased renal blood flow. However, higher blood pressure strains the afferent arteriole walls. Smooth muscle fibers in the afferent arteriole wall contract in response, narrowing the lumen. As a result, renal blood flow diminishes, lowering GFR to the prior level. When arterial blood pressure declines, smooth muscle cells become less strained and so relax. The afferent arterioles widen, kidney blood flow increases, and GFR rises. The myogenic process restores renal blood flow and GFR within seconds after a blood pressure shift.
Tubuloglomerular feedback is the second factor influencing renal autoregulation. To achieve autoregulation, the kidneys include a feedback mechanism that relates variations in sodium chloride concentration in the distal tubule. The macula densa is a collection of specialized cells that function as a feedback sensor. A high concentration of sodium chloride in the distal tubule implies a rise in GFR, whereas a low concentration indicates a decrease. The drop in sodium chloride concentration triggers a signal from the macula densa, which promotes dilatation of afferent arterioles and aids in the recovery of GFR to normal.
2. Tubular reabsorption and Tubular secretion
Tubular reabsorption is a highly selective process in which items are removed from tubular fluid and returned to the bloodstream. During glomerular filtration, all plasma elements except plasma proteins are filtered together through the glomerular capillaries. That is, in addition to waste products and surplus materials that the body has to expel, the filtered fluid contains nutrients (such as glucose and amino acids), ions (such as sodium, potassium, calcium, chloride, and bicarbonate), and other necessary chemicals. The important elements that are filtered are reintroduced to the circulation via tubular reabsorption. The nephron and collecting duct's second basic function is reabsorption. The urine contains just a small percentage, if any, of filtered plasma elements that are helpful to the body, as the majority have been reabsorbed and returned to the bloodstream. Of the approximately 125 ml of fluid filtered per minute, around 124 ml is reabsorbed.
Fluid passes along the renal tubule and into the collecting duct, and the tubule and duct cells discharge chemicals into the fluid. Hydrogen ions, potassium ions, creatinine, urea, and some medications like penicillin are examples of secreted substances. This is referred to as tubular secretion. tubular secretion has two possible outcomes:
- The secretion of hydrogen ion helps control blood pH.
- The secretion of some substances (such as urea, creatinine and certain drug) not needed by the body are removed from the blood.











Comments
Post a Comment