Reproductive system
The reproductive system is a group of organs and glands in the body that work together to facilitate reproduction. Males' reproductive organs include the testes, epididymis, vas deferens, and penis. Females' organs include the ovaries, fallopian tubes, uterus, and vagina. The male reproductive system's major role is to make and deliver sperm, whereas the female reproductive system is in charge of generating eggs, providing a proper environment for fertilization and fetal development, and giving birth. The reproductive system of humans consist of:
- Primary sex organs (gonads) which produce gametes and hormones
- Secondary sex organs which participate in reproduction
- Accessory sex organs that causes differences in the appearance of the two sexes
Ovaries and testes are the primary reproductive organs, sometimes known as the gonads. These organs produce eggs, sperm cells, and hormones. These hormones help to mature the reproductive system, develop sexual traits, and regulate normal reproductive physiology. All other organs, ducts, and glands in the reproductive system are classified as secondary, or accessory, reproductive organs.
Male reproductive system
The male reproductive system is composed of glands, their ducts, and supporting structures:
- The glands include a pair of testes, a pair of seminal vesicles, a pair of blbourethral or cowper's glands, and one prostate gland.
- Ducts of testes include a pair of epididymis, a pair of vas deferens,a pair of ejaculatory ducts, and one urethra.
- Supporting structures are divided into - a pair of spermatic cords and external, scrotum and penis.
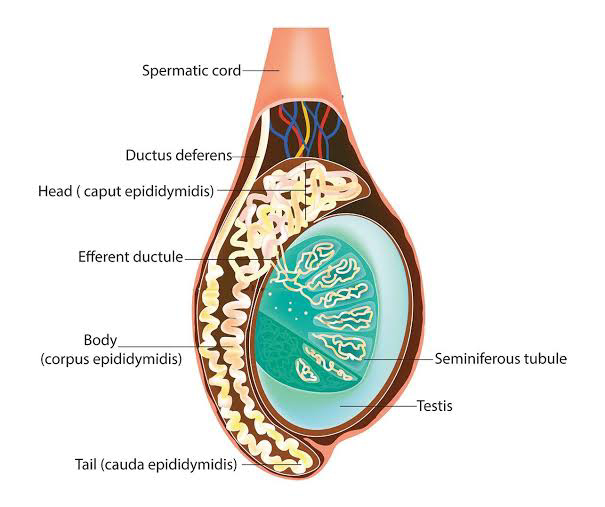
Testes
Male gonads, or testes, begin to develop high in the abdominal cavity, near the kidneys. They pass through the inguinal canal into the scrotum, a pouch that extends below the abdomen and posterior to the penis, in the last two months before or shortly after birth. Although the testes' placement outside the abdominal cavity may appear to make them vulnerable to harm, it provides a temperature around 3°C lower than normal body temperature. This lower temperature is required for the creation of viable sperm. Cryptorchidism occurs when a newborn's testes do not descend completely on one or both sides, leaving them in the abdominal cavity or inguinal canal.
Each testis is an oval structure. A strong, white fibrous connective tissue capsule called the tunica albuginea covers each teste and extends inside to form septa that divide the organ into lobules. Each testes has approximately 250 lobules. Each lobule has one to four strongly coiled seminiferous tubules that join to produce a single straight tubule that leads to the rete testes. Short efferent ducts leave the testes. Interstitial cells (Leydig cells), which create male sex hormones, are found between the seminiferous tubules of a lobule.
Functions of testes includes:-
- Production and storage of sperms that are viable
- Synthesis amd secretion of the androgenic hormone, testosterone.
Ducts of the testes : The fluid secreted by Sertoli cells exerts pressure on sperm and fluid, pushing it along the lumen of the seminiferous tubules and into a series of very short ducts known as straight tubules. The straight tubules connect to a network of ducts in the testis known as the rete testis. Sperm exits the rete testis and travels through a series of coiled efferent ducts in the epididymis before entering a single tube known as the ductus epididymis.
1. Epididymis - The epididymis is a comma-shaped organ about 4 cm (1.5 in) long that runs along the posterior margin of each testis. The epididymis is the site of sperm maturation, which occurs when sperm acquire motility and the ability to fertilize an ovum. This occurs over the course of around 14 days.
2. Ductus deferens - The ductus epididymis grows less convoluted and wider near the epididymis's end. Beyond this point, the duct is called the ductus deferens or vas deferens. The ampulla is the dilated end of the ductus deferens. During sexual stimulation, the ductus deferens transports sperm from the epididymis to the urethra using peristaltic contractions of the muscular coat.
3. Spermatic cord - The spermatic cord is a supporting element of the male reproductive system that emerges from the scrotum. It is made up of the ductus (vas) deferens, which ascends via the scrotum, the testicular artery, veins that drain the testes and transport testosterone into circulation (the pampiniform plexus), autonomic nerves, lymphatic vessets, and the cremaster muscle. The spermatic cord and ilioinguinal nerve both pass via the inguinal canal.
4. Ejaculatory ducts - Each ejaculatory duct is about 2 cm (1 in.) long and is created by joining the duct from the seminal vesicle with the ampulla of the ductus deferens.
5. Urethra - In males, the urethra is the shared terminal duct of the reproductive and urinary systems, acting as a channel for both sperm and urine. It is approximately 20 cm (8 in.) long and runs through the prostate, deep muscles of the perineum, and penis.
Accessory glands: The male reproductive system's accessory glands include the seminal vesicles, prostate gland, and bulbourethral glands.
1. Seminal vesicles - The seminal vesicles are saccular glands located posterior to the urine bladder. Each gland contains a small duct that connects to the ductus deferens at the ampulla, forming an ejaculatory duct that discharges into the urethra. The fluid from the seminal vesicles is viscous and contains fructose, which provides energy for my sperm; prostaglandins, which contribute to the motility and vitality of the sperm; and proteins that produce minor coagulation reactions in the semen following ejaculation.
2. Prostste glands - The prostate gland is a structure positioned directly below the urinary bladder. The prostate secretions are thin, milky-colored, and alkaline. They improve sperm motility.
3. Bulbourethral glands - The paired bulbourethral (Cowper's) giands are small, approximately the size of the penis, and are placed near the trase. In reaction to sexual stimulation, the bulbourethral glands produce an alkaline mucus-like fluid. This fluid neutralizes the acidity of remaining urine in the urethra, aids in the neutralization of the vagina, and provides lubrication for the tip of the penis during intercourse.
4. Seminal fluid - Seminal fluid, or semen is the fluid that is ejaculated at the time of orgasm. It is a slightly alkaline mixture of sperm cells and secretions from the accessory glands. Secretions from the seminal vesicles make up. about 60 percent of the volume of the semen, with most of the remainder coming from the prostate gland.
Hormones control:
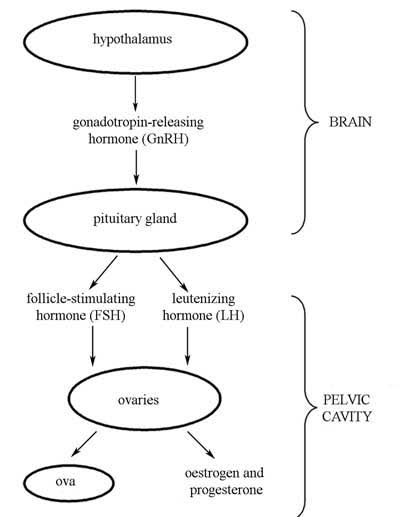
The hypothalamus has complete control over the testes' sexual function because it secretes gonadotropin-releasing hormone, or GnRH, which prompts the anterior pituitary to secrete gonadotropic hormones. Both males and females produce two gonadotropic hormones: follicle-stimulating hormone (FSH) and luteinizing hormone (LH). In males, FSH stimulates the creation of sperm in the seminiferous tubules, which also produce inhibin. In males, LH is also known as interstitial cell-stimulating hormone (ICSH) because it regulates testosterone production by interstitial cells located between the seminiferous tubules. All of these hormones work together in a negative feedback loop to keep sperm and testosterone production relatively consistent. The main sex hormone in males is testosterone, which is required for appropriate organ development and function. Testosterone is also responsible for the development and maintenance of male secondary sex characteristics during puberty.
Spermatogenesis:-
Spermatogenesis occurs within the seminiferous tubules. Spermatogonia, or immature germ cells found in the seminiferous tubule, divide by mitosis. Some of these cells begin meiosis I and become primary spermatocytes, after which they complete meiosis I and become secondary spermatocytes. The secondary spermatocytes then go through meiosis II to produce spermatids, which differentiate into spermatozoa (sperms) and are discharged into the lumen of the tube. Large cells extend from the tubule's periphery to the lumen and are interspersed with spermatogonia. These huge cells are Sertoli's cells, which support and nourish neighboring cells. During the differentiation process into spermatozoa, the majority of the spermatid cytoplasm is wasted as residual bodies, which Sertoli cells phagocytose. Spermatogenesis is also dependent on testosterone released by Leydig cells, which are positioned between the seminiferous tubules.
Every day, around 300 million sperm complete the spermatogenesis process. A sperm is around 60 micrometers length and comprises many features that are well-adapted for reaching and entering a secondary oocyte. The principal elements of a sperm are the head and tail; the sperm's flattened, pointed head is roughly 4-5 micrometres length. It has a nucleus with 23 extremely compacted chromosomes. A sperm tail is made up of four parts: the neck, the midpiece, the major piece, and the terminal piece. The neck is a restricted area just behind the head that houses centrioles. The centriole's microtubules make up the remainder of the tail. The midpiece contains spiral-arranged mitochondria that provide energy (ATP) for sperm motility to the site of fertilization as well as sperm metabolism. The main plece is the longest part of the tail, whereas the end piece is the terminal, tapering part of the tall.
Female reproductive system
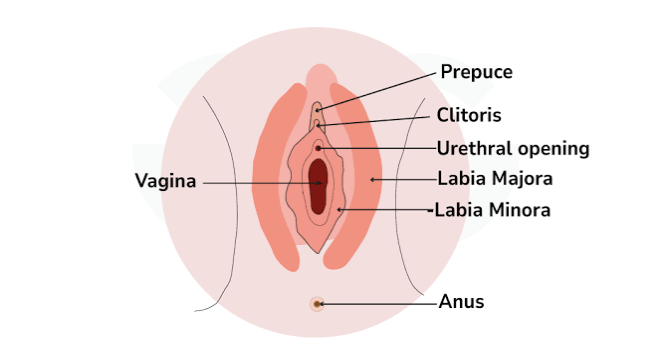
The female reproductive system's organs produce and sustain the female sex celis (egg cells or ova), transport these cells to a location where they can be fertilized by sperm, provide a favorable environment for the developing retus, move the fetus to the outside at the end of development, and produce the female sex normones. The female reproductive system consists of the ovaries, uterine (fallopian) tubes, or oviducts, the wterus, the vagina, and external organs known as the vulva or pudendum.
Functions of the female reproductive system are as follows:
The ovaries produce secondary oocytes and hormones, including progesterone and estrogens (female sex hormones), inhibin, and relaxin,
The uterine tubes transport a secondary oocyte to the uterus and normally are the sites where fertilization occurs.
The uterus is the site of implantation of the fertilized ovum, development of the fetus during pregnancy.
The vagina receives the penis during sexual intercourse and is a passageway for childbirth.
The mammary glands synthesize, secrete and eject milk for the nourishment of the newborn.
Ovaries
The two ovaries are the primary female reproductive organs, often known as gonads. The ovaries are situated in shallow depressions known as ovarian fossae, one on each side of the uterus, on the lateral walls of the pelvic cavity.
Histology of the ovary:
The germinal epithelium is a simple epithelium that covers the ovary's surface.
The tunica albuginea is a whitish capsule of dense irregular connective tissue found just under the germinal epithelium.
The ovarian cortex is located deep within the tunica albuginea. It comprises of ovarian follicles surrounded by dense irregular connective tissue with scattered smooth muscle cells.
The ovarian medulla is located deep within the cortex and houses blood arteries, lymphatic vessels, and nerves.
Ovarian follicles are made up of oocytes at various stages of development and the cells that surround them. When the surrounding cells form a single layer, they are called follicular cells; later in development, when they form multiple layers, they are known as granulosa cells. A mature (Graafian) follicle is a big, fluid-filled follicle that is about to break and release its secondary oocyte, a process known as ovulation.
A corpus luteum (also known as a yellow body due to the presence of lutein protein) includes the remains of a mature follicle following ovulation. The corpus luteum produces progesterone, estrogens, relaxins, and inhibins before degenerating into fibrous scar tissue known as the corpus albicans.
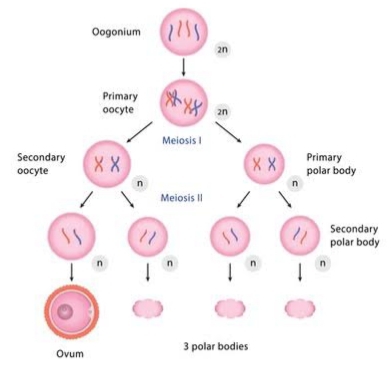
Oogenesis and follicular development:
The development of female gametes (eggs) in the ovaries is known as oogenesis. In contrast to spermatogenesis, which begins in males at puberty, oogenesis occurs in females before they are born. During early fetal development, primordial (basic) germ cells move from the yolk sac to the ovaries. The germ cells within the ovaries differentiate into oogonia. Oogonia are diploid (2n) stem cells that proliferate mitotically, resulting in millions of germ cells. The majority of these germ cells deteriorate prior to birth in a process known as atresia. A few, however, grow into giant cells known as primary oocytes, which enter prophase I of meiosis I during fetal development but do not complete the phase until after puberty.
At this stage of development, each primary oocyte is surrounded by a single layer of follicle cells. A primordial follicle is defined as an oocyte and the follicular cells that surround it. Gap junctions connect follicle cells to one other as well as the oocyte. Before birth, a small percentage of primordial follicles begin to mature into developing follicles. This oocyte has developed a thick zona pellucida and is surrounded by many layers of follicular cells (now known as granulosa cells) and a basal lamina, which separate it from the other cells in the ovary.
Following puberty, the hormones FSH and LH cause ovulation roughly once a month. The dominant primary oocyte completes meiosis I, producing a small polar body and a big secondary oocyte, which is the forerunner to the egg. The secondary oocyte then arrests at metaphase II. The follicle rapidly enlarges and ruptures at the ovary's surface, releasing the secondary oocyte, which is still enveloped by granulosa cells. If a sperm fertilizes the liberated egg within a day, it will complete meiosis II. The enormous secondary oocyte divides asymmetrically to create the mature egg (or ovum) and a second little polar body. Both polar bodies are tiny and will eventually degenerate. An egg, also known as an ovum, is a female gamete that can bond to sperm and become fertilized. An 'oocyte' is a developing egg that cannot yet bind sperm or become fertilized.
Hormones:
Follicle-stimulating hormone, luteinizing hormone, estrogen, and progesterone all play important roles in the regulation of the female reproductive system. At puberty, when the ovaries and uterus are developed enough to respond to hormonal stimulation, certain cues stimulate the hypothalamus to secrete gonadotropin-releasing hormone. This hormone enters the bloodstream and travels to the anterior pituitary gland, where it increases the secretion of follicle-stimulating and luteinizing hormones. These hormones, in turn, impact the ovaries and uterus, causing the monthly cycle to begin. Women's reproductive cycles last from menarche to menopause.
The monthly ovarian cycle begins with follicle development in the follicular phase, progresses to ovulation in the ovulatory phase, and ends with corpus luteum development and regression in the luteal phase. The uterine cycle occurs simultaneously with the ovarian cycle. The uterine cycle begins with menstruation in the menstrual phase, then moves on to endometrial repair in the proliferative phase, and finally to gland and blood vessel expansion in the secretory phase.
Menopause is when a woman's reproductive cycles finish. This period is distinguished by low levels of ovarian hormones and high levels of pituitary follicle-stimulating hormone and luteinizing hormone. The symptoms of menopause are caused by shifting hormone levels.
Uterine tubes - Females have two uterine tubes, called oviducts, which stretch laterally from the uterus. The infundibulum, a funnel-shaped part of each tube, is located near the ovary but opens into the pelvic cavity. It terminates with a fringe of finger-like extensions known as fimbriae. The ampulla is the largest and longest section of the uterine tube, accounting for around two-thirds of its length. The isthmus of the uterine tube is the more medial, short, thin, and thick-walled section that connects to the uterus.
Uterus - The uterus serves as part of the pathway for sperm deposited in the vagina to reach the uterine tubes. Anatomical subdivisions of the uterus include:
A dome-shaped portion superior to the uterine tubes called the fundus,
A tapering central portion called the body, and
An inferior narrow portion called the cervix that opens into the vagina.











Comments
Post a Comment